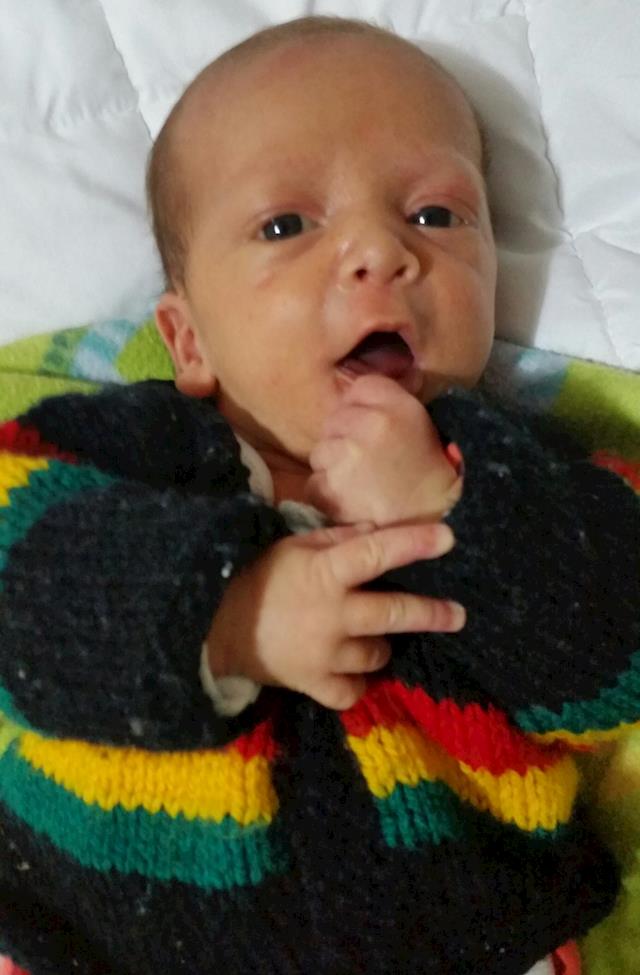
It's been touch and go over the last few weeks, but for now at least, baby Titaha is still alive.
Our baby's cardiologists were trying to figure out a way to surgically create a basic system of pumping oxygenated blood around his body, but because our baby's multiple congenital heart defects are so complicated, they decided that they need much better imagery and booked him in for some tests.
We found ourselves back in the Heart Ward 23b of Starship Hospital, where Titaha was put under anesthesia and had 3D ultrasounds, CT scans and a Cardiac Catheter, which is where they put a tube up one of the veins in his groin, all the way to his heart to check the pressures inside his right ventricle and the two different outlets coming off it.
He was also sent to the Renal unit for another type of catheter and xray to check that his urinary output was working correctly, as both of his kidneys have been dilated since before he was born.
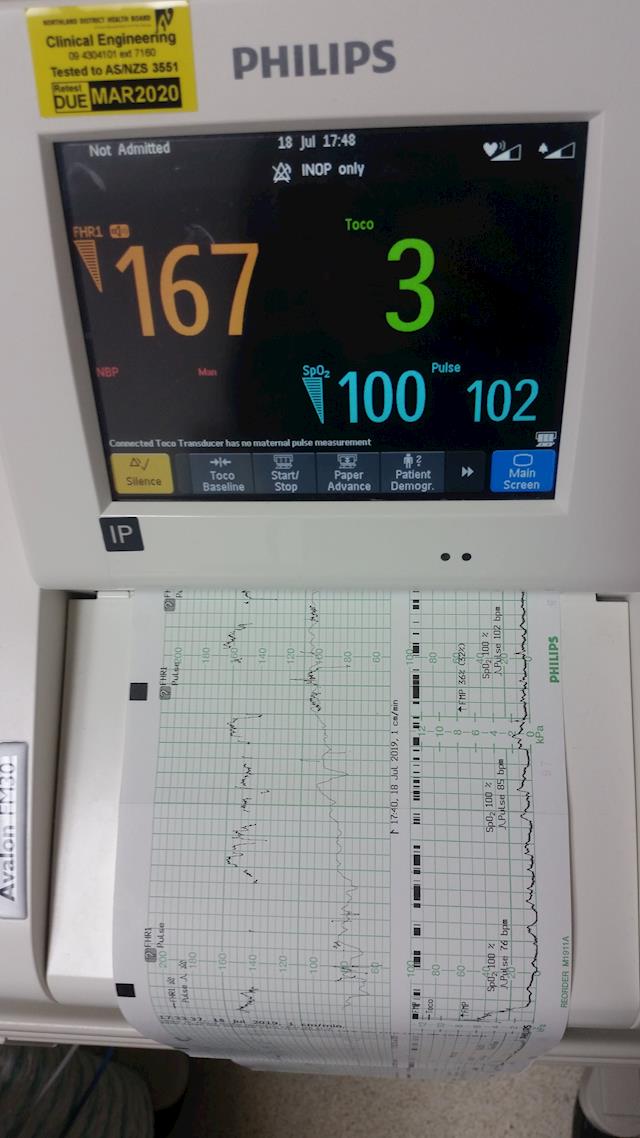
This was all very hard on our little man and he went down hill very quickly afterwards. His oxygen saturation levels dropped off the map a few times and he was put onto low flow oxygen to try and help him out. It's extremely difficult watching your little baby turn into a blueberry.
Unfortunately, he kept deteriorating over the next few days and his oxygen flow rate was increased, but by the time he was on 5 letres per minute, his oxygen saturations were no longer coming back up.
We really had to push for something to be done immediately, because we knew he wasn't going to make it through the week, let alone wait for his regular cardiologist and the only paediatric cardiac surgeon for the entire countries heart kids to return from their leave.
So a new team was quickly gathered together, who realized what we were saying was right. He would need some surgical help right away and thanks to finally having some proper data and imagery, they were able to make a spare of the moment surgical plan for Titaha.
A surgeon from Melbourne Children's Hospital in Australia happened to be in Auckland at the time and so they sent our baby into theatre for his first open heart surgery where they did 3 different procedures on that first day.
They cut out the Septal Wall between his Atriums, the top 2 chambers of his heart, put a banding around his Pulmonary Artery, that goes from his Heart to his Lungs and sewed in a Centrsl Shunt, which is a tube that goes between his Pulmonary Artery and his Aorta, which is the pipe that flows out to his body.
The next day, Starship Hospitals regular surgeon arrived back and she wanted to do some more adjustments on his heart, so Titaha was booked in for the following day, where he was wheeled back into theatre for further surgery. It was extremely hard watching him go through those double doors for the second time.
They loosened off the Banding on his Pulmonary Artery to let a little more blood flow through to his lungs and added another Band, this time around the Shunt that they had previously put in, to reduce the flow between his Pulmonary Artery and his Aorta.
After surviving all this, he was taken off his ventilation machine early and although we were told he would be kept sedated for a day or 2, he was allowed to wake up. This was quite a shock, but being able to give him a cuddle so soon after surgery was such a beautiful thing.
This first day of his recovery was very hard on him, but his numbers all looked good at that stage, so that night we decided to take the opportunity to try to get some rest. We made an arrangement with his bedside nurse to phone us if his numbers or any of his care plans should change.
They said that if he looked a little blue, they would put him onto low flow oxygen via simple nasal prongs, so we lay down for the first time in days, thinking we would be kept in the loop if something happened.
By the next morning, nobody had phoned us, but we found that his saturation levels had since dropped, he had fluid in his lungs and one of them had collapsed during the night. They had him on a high flow oxygen machine with PEEP to help keep his Avioli open and push some of the fluid back through into his lung tissue. They also added another medication to help get rid of the excess fluids.
He has been in a lot of pain and after the Morphine had worn off, he was only given 4 hourly doses of Pamol for pain relief. It was a long hard day for him and us, as we begged all day for some more pain relief to be given to him, so that he would be able to get some much needed healing rest.
Eventually, he was given a dose of morphine and then he went straight to sleep. We have been clearing the bubbles from his mouth with a cloth and are now simply too scared to leave his side, in case something happens in the night and nobody calls us again.
This surgery was not part of his cardiology plan and he will still require at least 2 more open heart surgeries and possibly a Heart transplant to create a long term working systemic blood flow. It's so hard not knowing if our precious little baby boy is even going to make it through another night or not.
Thanks again for everyones donations. It means a lot and helps with some of his very expensive equipment we have had to buy for him. We are still desperately trying to save for his next medical equipment and supplies, as well as being likely to need to travel overseas eventually for his transplant.
Fingers and toes are crossed that he makes it through the next stage.